A workshop repair manual is an indispensable tool for car owners, mechanics, and automotive enthusiasts. These comprehensive guides provide step-by-step instructions, technical specifications, and illustrations for maintaining, diagnosing, and repairing vehicles of various makes and models. In this article, we will explore the significance of workshop repair manuals, how they assist individuals in the automotive world, and where to find them.
When it comes to vehicle maintenance and repairs, having a workshop repair manual at your disposal can truly be the ultimate resource. Gone are the days of relying solely on mechanics and spending a fortune on simple fixes. With a detailed repair manual, you have the power to tackle minor issues yourself, saving time and money in the process. Not only does this empower you as a car owner, but it also allows you to develop new skills and deepen your understanding of how your vehicle functions.
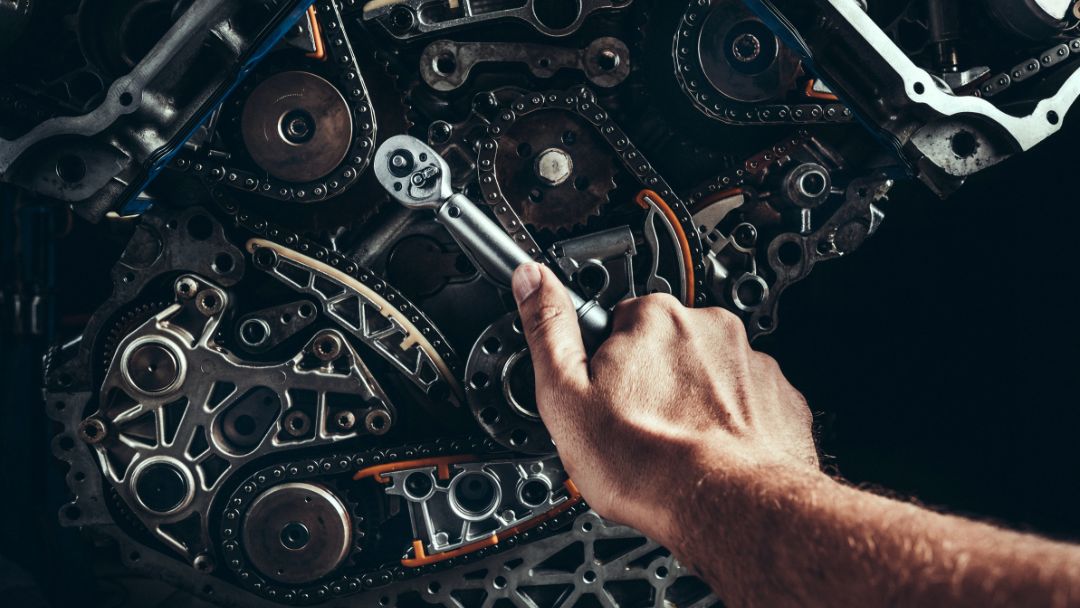
One of the key advantages of using a workshop repair manual is that it provides step-by-step instructions for various tasks. Whether you’re looking to replace a spark plug or troubleshoot an electrical issue, these manuals guide you through each stage with clear illustrations and concise descriptions. Furthermore, they often include useful tips and tricks that can save you hours of frustration. Rather than relying on trial and error or online forums with varying opinions, having a reliable source like a repair manual ensures accuracy in your repairs.
Beyond providing technical guidance, workshop repair manuals also offer insights into preventive maintenance. They outline recommended service intervals for different components of your vehicle, helping you stay proactive in keeping everything running smoothly. By following these guidelines and performing regular check-ups as suggested by the manufacturer, not only will small issues be detected early on before they escalate into major problems but your overall vehicle performance will improve as well.
What is a Workshop Repair Manual?
A workshop repair manual, also known as a service manual or repair guide, is a detailed document that offers comprehensive information on a wide range of automotive tasks. These tasks include routine maintenance, diagnostics, and complex repairs. Workshop repair manuals are created by vehicle manufacturers or third-party publishers and are designed to ensure that repairs and maintenance are carried out accurately and efficiently Workshop Repair Manual.
How a Workshop Repair Manual Assists Automotive Enthusiasts and Mechanics
A workshop repair manual is an invaluable tool for a variety of individuals and purposes:
- Professional Mechanics: Certified technicians and mechanics rely on these manuals to ensure accurate, manufacturer-approved repairs and maintenance for a wide range of vehicles.
- DIY Enthusiasts: Automotive enthusiasts who prefer to work on their vehicles use these manuals as a valuable resource for tasks such as oil changes, brake repairs, and more.
- Troubleshooting: Detailed procedures and wiring diagrams in these manuals are crucial for diagnosing and resolving issues efficiently, saving both time and money.
- Restoration Projects: Classic car owners and restoration enthusiasts find these manuals essential when working on vintage and antique vehicles.
- Educational Resource: Workshop repair manuals also serve as educational resources in automotive schools, training centers, and technical training programs, providing valuable information to future mechanics and technicians.
Features of a Workshop Repair Manual
A workshop repair manual comes with a range of features and benefits:
- Detailed Procedures: They provide step-by-step instructions for various automotive tasks, ensuring precision and accuracy.
- Wiring Diagrams: These manuals include wiring diagrams and electrical schematics, which are essential for diagnosing electrical issues.
- Parts Catalog: Some manuals include parts catalogs, making it easier to identify and order the correct replacement parts for a vehicle.
- Maintenance Schedules: Many workshop repair manuals offer recommended maintenance schedules, helping vehicle owners keep their cars in optimal condition.
Where to Find a Workshop Repair Manual
A workshop repair manual can be sourced from various channels:
- Official Manufacturer Websites: Some vehicle manufacturers offer digital versions of their workshop repair manuals for purchase or free download on their official websites.
- Third-Party Publishers: Independent publishers often create and sell workshop repair manuals in print and digital formats.
- Online Communities: Enthusiast forums, automotive communities, and websites dedicated to specific car models may provide digital copies or links to these manuals.